How to Build a High-Authority Recruiting Agency That Attracts $20K/Month in Commissions on Autopilot …
…WITHOUT cold calling, manual prospecting, or having to quit your job
What Does Recruitemy Do?
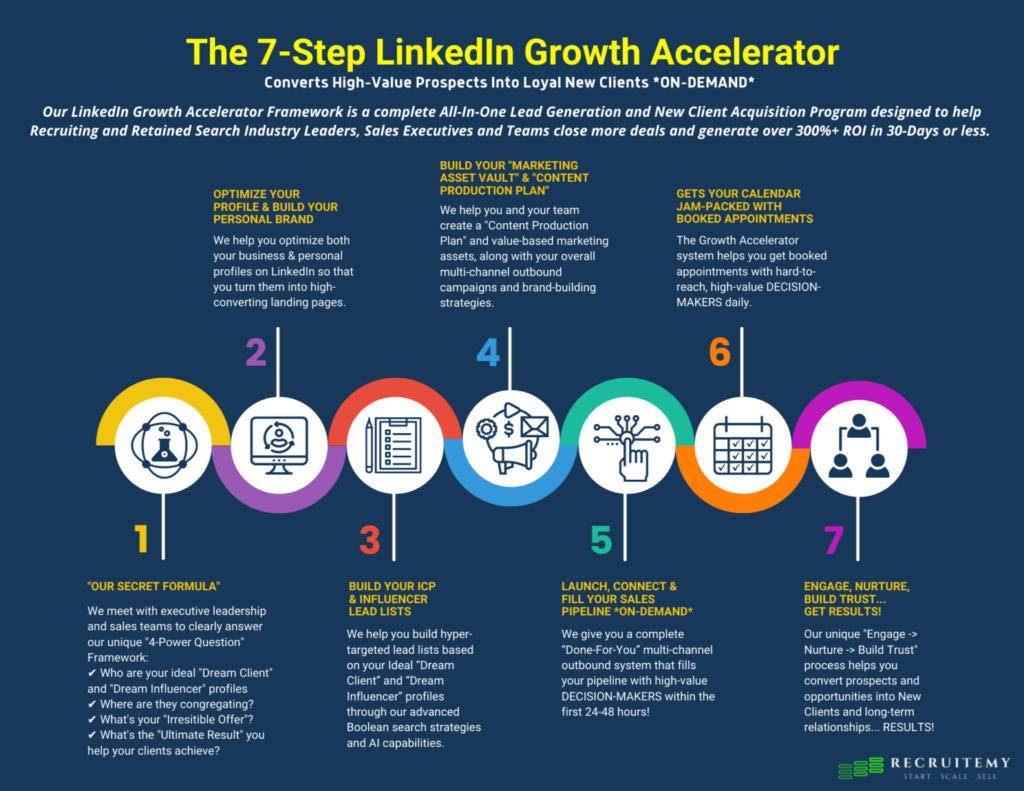
Recruitemy gets entrepreneurs laser-focused on ATTRACTING inbound QUALIFIED Leads utilizing Personalization, 1:1 Video plus Automation from A-Z.
Who Does recruitemy Help?
Recruiters, Staffing Owners, Staffing Sales Execs, Retained Executive Search, Contingency, Direct-Hire, Engaged Search, Contract and Contract-to-Hire
How Does Recruitemy Help?
Most staffing entrepreneurs (established or brand new). They’re just following the old-school methods they were taught. It’s not their fault though. Still trading time for (not enough) dollars. Chained to their business in the day-to-day. Not able to see the wealth of opportunity at their fingertips and the new way of doing things.
Recruitemy Makes You....
The rarest breed of recruiting and staffing professionals, a hyper-profitable entrepreneur. They’re constantly pioneering innovations in marketing, sales, and management. Disrupting a 157.8 billion dollar market. You wont find them in the traditional recruiter habitat. They are unorthodox, advanced, and always winning.
- Copyright 2026
- Recruitemy | 400 N Tampa St, Tampa, Fl 33602
- Contact: info@recruitemy.com
- 813.928.2015
This site is not a part of the Facebook website or Facebook, Inc. Additionally, this site is not endorsed by Facebook in any way. FACEBOOK is a trademark of FACEBOOK, Inc.
DISCLAIMER: The results stated above are my personal results and the results of my clients. Please understand our results are not typical, we’re not implying you’ll duplicate them (or do anything for that matter). We have the benefit of having gone through much training, trial, and error for years, and have an established following and history as a result. The average person who buys any “how to” information gets little to no results. We’re using these references for example purposes only. Your results will vary and depend on many factors …including but not limited to your background, experience, and work ethic. All business entails risk as well as massive and consistent effort and action. If you’re not willing to accept that, please DO NOT GET THIS TRAINING. By submitting your email address on this website, you are authorizing our company to send you informational and promotional messages via email, phone calls, and text messages.